
Gait Harness System
Publications, Case Studies & Press Releases
Publications, Case Studies & Press Releases
Gait Harness System Publications, Case Studies & Press Releases
The Gait Harness System provides therapists and patients with the tools they need to accomplish a necessary step in the recovery process.
Recovery focused therapy outcomes
The Second Step Gait Harness System (GHS) is a unique, all-in-one standing frame and walking frame, providing safety, ease of use, comfort, security, and great versatility. When donning the Gait Harness and supported within the GHS, the user cannot fall.
GHS products help:
- improve balance
- increase stability
- improve muscle strength
- increase core & trunk control
- improve circulation
- promote bone & musculoskeletal health
- improve range of motion
- increase independence
- improve positive therapy outcomes
- support faster recoveries
Understanding Second Step Gait Harness System products and their applications to the life and health of any patient is due in part to the implicit design of the System, and then to the application of physical therapy principles and the fundamentals of physiology, biomechanics and neurology.
The Gait Harness System provides therapist and patient with the tool they need to accomplish a necessary step in the recovery process. No other system provides the same combination of therapeutic advantages, safety and ease of use.
The System also allows for a creative, responsive and innovative approach that considers the many physiologic, biomechanical, and biochemical factors, as well as the individual’s opinions, emotional and spiritual needs.
The Gait Harness System allows for a therapist to efficiently address the needs of patient from the acute to the chronic setting. Therapists have seen an undeniable need for the Gait Harness System, and a recovery focused ideology to be implemented throughout a patient’s continuum of care.
The safety of the Gait Harness System benefits clients, caregivers, and practitioners alike. Many of those using the Gait Harness System also realize that greater savings can be realized from longer, recovery-focused care following the initial injury, rather than repeat care, which targets adaptations and accidents later in life.
Below browse publications, case studies, and press releases regarding Second Step products.

PROGRESSION OF AMBULATION IN A PERSON WITH INCOMPLETE PARAPLEGIA USING AN OVERGROUND HARNESS SUPPORT FRAME
Camacho MA, House MJ, Shields RK. University of Iowa Hospitals and Clinics and the University of Iowa Graduate Program of Physical Therapy and Rehabilitation Science, poster presented at APTA CSM 2003
PURPOSE: This case report describes a novel over ground gait training system that was used to facilitate functional ambulation in a person with incomplete spinal cord injury.
SUBJECT: The subject was a 22-year old female who sustained an incomplete spinal cord injury eleven months prior to initiation of outpatient therapy. The spinal cord was injured at the fourth thoracic level and caused residual diminished strength, proprioception, light-touch senses below the level of injury and absent pain and temperature senses. The American Spinal Cord Injury Association (ASIA) functional score was graded as C. The subject was on a prescription medication to manage spasticity of the lower extremities. The patient also reported her gait had remained the same over the last several months.
METHODS: The subject received physical therapy services for an hour and a half 3 times per week for 6 weeks. The primary intervention was supported gait training provided by the Second Step ™ system, which consisted of a wheeled frame with harness support for over-ground walking. Other interventions included lower extremity stretching and strengthening exercises. Pre-treatment and post-treatment measures were (1) 50-foot walk speed (2) Sit to stand height from a high/low mat with use of standard walker and one hand support on walker, (3) level of assistance needed for gait, and (3) a modified Quality of Life SF-12 Questionnaire (Shields 2002).
ANALYSIS: The percentage change in walking speeds, ability to rise from a chair, level of assistance, and the modified SF-12 scores was calculated before and after 6 weeks of the supported walking program
RESULTS: The subject demonstrated a 62 % decrease in the 50-foot walk speed from 170-seconds to 65-seconds following the training with the over ground harness system and required 20 % less assistance. The subject’s ability to rise from a progressively lower seated position improved by 16% from 25 inches to 21 inches. The patient’s perception of health quality remained over this 6-week time.
CONCLUSION: This subject demonstrated improvement in gait velocity, assistance needed, and ability to rise from a seated position after using the Second Step ™ gait training device. However, the improved walking did not reach a threshold to cause an improved perception of health quality.
RELEVANCE: Use of a gait training device, such as the Second Step ™, provided an individual with incomplete spinal cord injury the opportunity to walk with partial support of body weight without utilizing the more expensive suspended treadmill systems. Over-ground walking with this device may be facilitating the use of Central Pattern Generators for improved reciprocal gait ability. The results of this study have important practical and economic implications for the therapist designing a rehabilitation program for individuals with SCI.
Dr. Richard K. Shields PT, PhD
Chair of the Department of Physical Therapy and Rehabilitation Sciences at the University of Iowa Carver College of Medicine; Researcher & Professor; Director of Human Movement Control/Performance Laboratory; Member of the Board of Trustees for the Foundation for Physical Therapy
SECOND STEP GAIT HARNESS SYSTEM
AS COMPARED TO BODY WEIGHT SUPPORT SYSTEMS
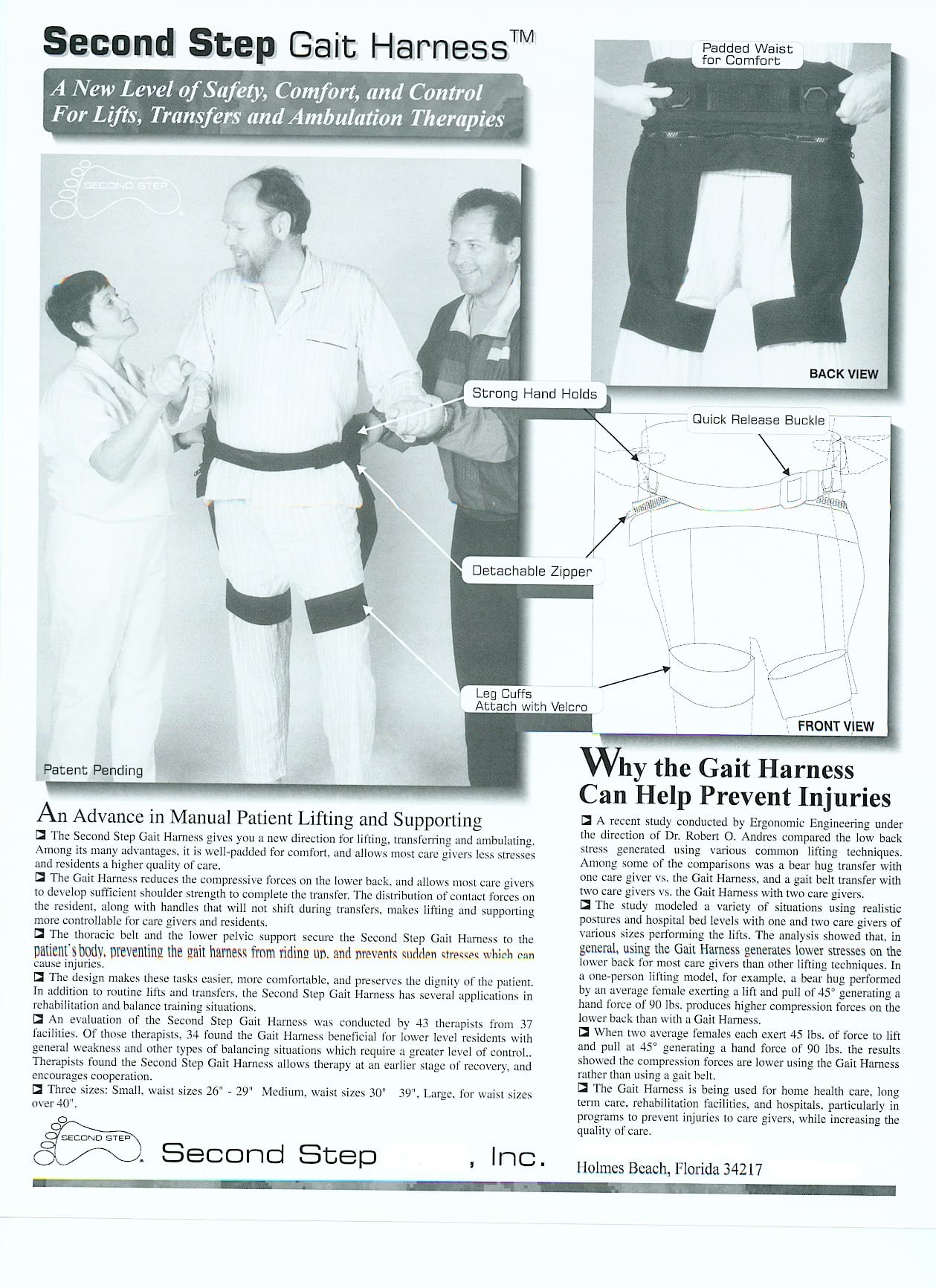
The Second Step Gait Harness System (GHS) ambulator has several distinctions that make it unique when compared to body weight support systems.
First, the GHS does not directly off-load the individual’s weight. Weight reduction (if needed) is performed actively by the individual in the System. Most individuals will not have home access to a body weight support treadmill training system, but may be able to implement an over-ground system that allows for the efficient reinforcement. I use the Gait Harness System, which does not directly offload weight, to accomplish this reinforcement (the individual offloads as needed or instructed).
Second, the harness used in the GHS directs supportive forces (or fall recovery forces) through a much larger surface area on both thighs. Other over-head harnesses direct these forces through the sensitive pubic area, which often leads to decreased treatment time and intensity.
Lastly, the GHS allows for reinforcement of newly learned gait patterns in a real-world situation. I have implemented this technique with several incomplete Spinal Cord Injury individuals and have had great success in regards to gait speed and distance. This is a very beneficial and much needed adjunct treatment paradigm, and accentuates body weight support treadmill training. Body weight support treadmill training, in general, has shown a benefit of retraining central pattern generation and the ensuing stepping pattern.
Body weight support treadmill training can be difficult and labor intensive. For body weight support treadmill training to be effective, any progress made needs to be safely reinforced with over-ground training.
The GHS allows you to safely transfer and reinforce this progression to various land-based gait training activities. Reinforcement of the various qualities of gait during land-based activities is a must for the activity to become functional.
Lead Physical Therapist, Center for Spinal Cord Injury Recovery, Rehabilitation Institute of Michigan; Level Eleven Physical Therapy Clinics Founder; Clinic Director, Oakland Orthopaedic Physical Therapy Institute
ADDRESSING RESIDENT MOBILITY AND FALL PREVENTION:
A CLINICAL PERSPECTIVE WITH GAIT TRAINING
An integral component of the care of residents or patients in long-term care facilities is the maintenance and restoration of functional activities. Ambulatory goals are a central component for most residents. In therapeutic or restorative gait programs, the challenge is to provide a safe and effective method for both resident and caregiver. Falls can be a devastating problem for the resident, caregiver and the risk management in a facility. Advances in ambulatory and support devices provide a safe and effective method for mobility of the resident that can make a significant impact on the overall health of residents, caregivers and the cost effectiveness of treatments in facilities.
Falls in nursing homes and long term-care facilities as noted by the National Center for Injury Prevention and Disease Control are a serious problem with approximately 50% of the 1.5 million residents nationwide falling at least once per year. These falls occur in part because the residents in our facilities are in need of our help. They are often older, frailer, more cognitively impaired than those living outside long-term care facilities. For these reasons, residents being transferred or ambulated, may “give way” suddenly, without warning and resulting in a fall unless we are properly positioned and ready for this event. In the Nursing Home Long Term Care June 2000, article on Improving Resident Transfers, Wood et al., point to improper training for manual lifting techniques with under arm holds as a major culprit for injuries. The training of the clinical/caregiver staff was addressed and the cost savings relating to proper training was discussed in detail. The most common causes of nursing home falls are weakness and gait problems, which accounts for 24% of the falls. Environmental hazards (wet floors, lighting etc.), medications, difficulty in transferring and foot care are some of the other causes.
Identifying predisposing factors and assessing resident-caregiver risk can assist in forecasting fall risk of the resident, the caregiver and the facility in regards to mobility and fall prevention.
Predisposing factors with falls as it relates to the resident may be weakness and gait problems, poor general health, impaired mental status possibly influenced by medications and their emotional status. Predisposing factors for falls as it relates to the caregiver may be improper training in both transfers and the use of transfer and ambulatory equipment, and physical factors such as a disparity between the size of the resident and the size of the caregivers. The facility’s predisposing factors include limitations of equipment used or provided that reduces the stresses during lifting and supporting residents. Environmental factors that can lead to falls are lighting, flooring and other design issues. The challenges encountered by caregivers while assisting residents with mobility and transfer activities are some of the most difficult challenges in long-term care facilities today, as the residents can suddenly “give way.” If a fall occurs, the mutual trust that is necessary for advancement in therapy programs is strained.
From a clinical perspective, the fall and mobility issues for residents should address those factors that can be influenced through implementation of products and services that will most effectively address the major causes of falls while maximizing the benefits of mobility for residents.
Researchers in the area of physical therapy and mobility are looking at new ways to address these areas and they have encouraging news. New technologies are emerging in the industry such as such as ambulator-gait harness systems have a significant impact with regards to clinical experiences. These systems provide for safe, effective and dynamic gait training programs that can be integrated into all ambulatory and transfer needs of the facility. One such system is the Second Step, Inc. Gait Harness System (GHS). The system is composed of a gait harness and ambulator. The gait harness designed to reduce the stresses/compressive forces on the lower back of the caregiver during gait training activities.
Dr. Robert Andres has written about the uses of gait harness systems. In a study he modeled a variety of situations using realistic postures with caregivers using gait harnesses. Other researchers also relate to finding safety solutions for Mobility and Fall Prevention as described in The Isernhagen Work Report, Fall 2000, the Ergo Focus identifies that the harness distributes the patient’s weight, allowing caregivers to manage residents more easily and safely. The gait harness also provides the caregiver a unique ability to control the lower half of the resident’s body during transfers providing substantially improved manual control and assist of the resident as needed. Through secure handholds built into the harness, caregivers can be sure to position themselves properly with both single and two-person assistive activities. The use of the gait harness in weight-bearing assistive programs addresses both mobility and safety issues effectively.
The following therapists’ clinical experiences identify resident mobility outcomes that address many of these key factors in fall prevention with gait training. According to Linda Horn, PT, NCS, the inpatient physical therapy coordinator for St. Agnes Healthcare, Baltimore, Maryland, a 407 bed Integrative Health Care Facility, once the resident is properly placed in the gait harness, they can be transferred into the ambulator for mobility activities. When the resident is properly secured in the GHS, the resident is completely supported without the need for the caregiver to hold onto the resident directly. This eliminates the risk of injury from the resident suddenly “giving way” and falling to the floor. Since the resident is in a stable and secure environment, mobility activities can be performed relatively hands free for the caregiver. Linda states “the resident’s confidence is then restored, which can be a huge barrier removed,” thus allowing the therapist to concentrate on fine-tuning the resident and addressing weakness and other gait deviations.
The clinical perspective from Healthsouth Rehabilitation in Tampa, FL, where patients whose diagnosis range from Traumatic Brain Injury (TBI) to post-operative total joint replacements have demonstrated functional advancement in weight-bearing activities at faster rates with a higher level of functional performance. Mutual trust between the resident and therapist while being held/supported with the GHS is enhanced and more productive therapy sessions can follow. The clinician can advance the therapy program by performing tasks that are above the current functional level of the resident and yet not increase the risk of injury to either the caregiver or resident.
Clinicians progressed another patient, who in five years of on again off again rehabilitation, failed to develop independent ambulatory capabilities for even short distances. The therapist integration of the GHS with this resident made tremendous progress and independence with ambulation for moderate distances of 200 to 300 feet through aggressive therapy in restorative gait training programs. The system allowed the therapist to use his hands to resist or assist the patient despite her difficulties relating to balance control. For example, the therapist stood a short distance behind the patient and resisted her lower extremities. Resistive tubing was utilized to provide resistance to the thigh to enhance motor recruitment and facilitate normal patterns of movement without the need to hold on to the resident. This allowed the resident to receive truly skilled hands-on care for more progressive therapy sessions by concentrating on specific areas such as neural programming and coordinate task in standing. The therapist noted an increase in resident motivation and confidence as therapy progressed. Simple task such as backward walking could be performed with the therapist focused on retraining the movements and assisting or resisting without fear of the resident falling. At Providence Benedictine nursing center, Mt. Angel, Oregon, Theresa Raudsepp, MSPT, reports that one of her residents with a brainstem CVA utilized the GHS during her stay. Emphasis was placed on symmetrical stride length and cadence with the goal of normalizing her gait. Another resident with a diagnosis of left hemiplegia and right total knee replacement was treated with a therapy program that included GHS. This allowed the caregiver to address both the complications of his hemiplegia while at the same time restoring the strength and function of his lower extremity in standing. The system provided the resident with a secure environment to ambulate. This enhanced his muscular recruitment and the resident soon overcame his foot drag.
At IHS of Braden River, Bradenton, Florida, a 208 bed SNF, clinicians indicate therapy time for a nursing home resident with TBI, was shortened by 6 weeks after the introduction of the GHS. This resident lacked enough motor control to ambulate safely in a walker without assistance. The resident was able to quickly gain self-control of her gait in part because she could not rely on someone else to support her and lean on the caregiver. She gained confidence quickly and was soon able to ambulate, perform higher-level coordinative activities such as catching and throwing a ball and build her endurance through walking in this system.
Liza Chuanico Bolle, RPT follows an integrative approach with their restorative gait training programs. Favorable intervention efforts are getting the results that caregivers are looking for with Mobility and Fall Prevention as it relates to gait training. One 200 lb. TBI resident previously ambulating using a rolling platform walker 200-300 feet for 30 minutes, required 2 caregivers assistance due to a tendency to lean to the right side with the right leg buckling under him. GHS has assisted the patient to assume a more upright and symmetrical position through arm supports and has cut ambulation time to 5 minutes. This reduced assistance to 1 person per resident and restorative aid feedback, the system provided a secure and stable environment allowing overall improvement in this program.
These programs benefit residents, caregivers and the facility. They reduce the risk of falling by restoring and maintaining resident muscle strength and control, improving range of motion, joint nutrition and function, improving circulation, maintaining bone density and increased alertness. In addition, residents have the psychological benefit of increased self-esteem from actively participating in their own care with a greater degree of independence. The entire health care team benefits from greater resident physiological improvements, which prevents falling injuries and a reduced risk of injury to caregivers since these systems provide a safe environment for the resident during ambulatory activities.
In summary, clinicians indicated very promising outcomes in relation to fall prevention and mobility. The challenges that nursing home facilities are confronted with in relation to complex and difficult areas are being met with very favorable intervention efforts. Researchers and therapists offer evidence that options exist that provides encouragement. Implementing effective systems and programs within the long-term care facility can prevent injuries that are fall related while increasing opportunities for your facility’s mobility outcomes.
Impact Health Clinic Founder & Owner, Palm Harbor FL
References
Andres RO. Resident transfer: Scientific testing begins. Nursing Homes/Long- Term Care Management 1998; 47-60.
Baker SP, Harvey AH. Fall injuries in the elderly. Clinics in Geriatric Medicine 1985; 501-7.
Bureau of Labor Statistics, US Department of Labor, Washington D.C. (1995, April). News (USDL-94-600)
Ejaz FK, Jones JA, Rose MS. Falls among nursing home residents: An examination of incident reports before and after restraint reduction programs. Journal of the American Geriatric Society 1994; 42(9):960-4.
Rubenstein LZ. Preventing Falls in the nursing home. Journal of the American Medical Association 1997;278(7):595-6
Rubenstein LZ, Robbins AS, Schulman BL, Rosado J, Osterweil D, Josephson KR. Falls and instability in the elderly. Journal of the American Geriatric Society 1988;36:266-78.
Tinetti ME, Speechly M. Prevention of falls among the elderly. New England Journal of Medicine 1989;320:1055-9.
Nursing Homes Magazine, February 2001, “Gait Training to Improve Resident Mobility” Read here
Case Studies
Visit GHS Comebacks and Video Gallery to watch case study videos in action.
Knute M. & Marlene M. Grace Center for Adult Day Services is an adult day health center located in Corvallis, Oregon. We have been using the Second Step Gait Harness System (GHS) ambulator since late 2005, and we have seen great results with several of our participants (clients).
Of particular note is the experience of our youngest participant, Knute M., who is now 35 years old. When Knute was 11 years old, he had a traumatic brain injury from a MVA and had never walked after that accident. In February 2006 Knute began walking in the Gait Harness System twice a week at Grace Center. This was a “dream come true” for this young man! Knute began walking only a few feet, and had worked his way up to 150-200 feet by October of 2007. As of January 2008, he was routinely walking 400-450 feet in the GHS. Staff allowed Knute to increase his walking distance to 500 feet, keeping in mind a focus on improving and controlling his gait technique, in addition to his stamina and distance.
By October of 2008, Knute was regularly walking over 1,000 feet per session. He can now use the GHS with the assistance of only one staff member who walks behind the ambulator. Knute’s posture, balance, and gait have improved greatly with practice and coaching. Staff members encourage him to bring his shoulders backward, “tuck under your buns” (tilt hips & pelvis forward), and take smaller steps. Knute’s thigh muscle strength and size have increased so much that he now needs a larger size harness! His home caregiver says that his is much stronger and better able to assist with transfers. At his most recent care conference, some improvements were also noted in the Communication, Socialization, and Problem-Solving ratings of the FIM (Functional Independence Measure).
The Second Step GHS has also allowed several of our other participants who had stopped walking to regain their ambulatory ability. We have found it is especially useful for hemiplegic participants who have very poor balance and are therefore at high risk for falls. The GHS prevents injury not only to the participants but also to the staff members who are walking with them.
The Second Step GHS has also allowed Marlene M., a 50-year-old participant with cerebellar degeneration and severe balance disturbance, to walk at Grace Center. By mid-October 2007, she was walking about 100 feet in the GHS. As of January 2008 she had increased her distance to 125-175 feet per day. By May 2008, she was walking 200 feet per day. As of October 2008, Marlene is now walking 250 feet per session. This has greatly improved her strength and stamina, making chair and wheelchair transfers much easier for her. Marlene’s gait has also become more normal and her turns in the ambulator are smoother. She feels much more confident doing independent transfers both at the Center and in her home, and has commented that her legs are stronger, and her trunk control is getting better.
We love our two Second Step Gait Harness Systems and highly recommend them to other health care providers!
–Cheri Babb RN, Executive Director, Grace Center for Adult Day Services, Corvallis OR
I use the GHS with a variety of patients. The combination of the GHS frame and supportive belt and thigh straps allow me to progress a patient from a very low level up to higher level gait training and more advanced physical activities. I can start with patients in the harness on the edge of a mat table and am able to facilitate more trunk control/initiation for activities such as sit-to-stand. The GHS walker allows me to then safely progress on to gait activities including varied pace, increased stride length, visual scanning and multi-distractions.
The big benefit of the GHS is that it allows me to do these activities in a very, very safe environment for myself and the patient. The GHS will not allow the patient to fall. It allows the patient to “take a break,” by just sitting down in a relaxed position without me needing to transfer them to a chair or mat table or have myself or a second person drag a wheelchair behind. With patient in the GHS, I can also safely do a variety of challenges with TheraBand, ball tossing, sensory motor, and proprioceptive training, while standing or ambulating, as the patient is completely secure.
Since nearly all of my work is without an aide, the GHS is like another set of hands and probably provides just as much safety as an aide would.
Floor transfer training is always challenging for both the patient and the therapist, but the belt support system used outside the GHS frame is an excellent way to do this exercise with increased control and safety.
The GHS has helped me develop more techniques that have improved the way we treat our CVA patients. Adjusting the height of the GHS upper support panel helps us work on trunk control. Adjusting the straps allows us to encourage weight shifting or weight bearing to the involved side. It also enables both our hands to be free to facilitate the lower extremity in standing, without worrying the patient will fall.
I have found particular success with the frail, sedentary elderly patients who have developed balance difficulties and an extreme fear of falling with any anterior translation of their body. They typically have slow shuffling gait with poor stride length, overdependence on their upper extremities, poor trunk control and lack of endurance from their sedentary existence.
The braking system is nice. It allows us to progress the patient from ambulation in-line to requiring lateral control, and frees them to move side-to-side or any 360-degree direction.
An interesting case was a young patient who suffered a brain injury and wanted to get back to his soccer and sports activities. He initially was not able to do these activities due to his spasticity and coordination issues. By progressing him in the GHS, where he was allowed to safely make mistakes, he was able to eventually skip, jump, and do single leg activities safely. He was delighted that he could return to some of his favorite activities again.
I believe the GHS would be beneficial in the home. It would help with carry over and safe household ambulation, decreasing risk of injury for patient and caregiver.
We had one patient who was severely ataxic and could not walk safely. When she came to us she had not been upright, except for assisted transfers, for over a year and required over 50% assistance in all daily living activities. Walking was out of the question as it required maximal assistance, and was completely unsafe. We placed her in the GHS and she was eventually able to walk with the assist of only one person safely. She was able to increase her heart rate and developed some cardiovascular fitness. She also started to lose weight. Her coordination did improve, and she felt happy daily. After she was discharged she unfortunately went back to a completely sedentary life style in sitting because she had no safe equipment to use for upright activities and ambulation at home. She was at risk for contractures and developed weakness, became deconditioned and gained a lot of weight, making mobility even more difficult for her caregiver. The GHS would have been a perfect home device, but Medi-Cal would not cover the cost of this very useful equipment for her.
The GHS has enabled me to do advanced activities in a very safe (for both myself and the patient) environment. It has also been an extra set of hands and probably paid for itself within a few months of use.
–M. Rosalia Arellano MSPT, Scripps Mercy Hospital, Outpatient Neuro Rehabilitation Department, San Diego CA
I have experienced positive outcomes with using the Gait Harness System (GHS) with the TBI population. The device allows for early gait training which helped patients feel successful in working towards their goals of independent ambulation. The GHS is a safe way to work on motor control/motor learning while the therapist can focus on facilitating a more normal gait cycle. I have also found the GHS promotes a faster gait velocity which is difficult to obtain with over the ground ambulation (without the use of a treadmill). The benefits I have noticed are the following:
-comfortable harness that the patient can take sitting rest breaks in
-safe way to provide early gait training
-allows the therapist to focus on facilitation techniques vs. holding a patient upright
-encourages independence
-can be used outdoors to help people psychologically
-can ambulate further distances and work on endurance (less therapist fatigue)
-can be used to perform sporting activities to work on balance/strength
Many brain injured patients have poor insight and are impulsive, therefore the GHS would be a good option for a patient at high risk for falls to walk safely with trained family/staff members. I can also see the potential benefits of using the GHS with amputee patients who are fearful of falling and can promote less dependence on the parallel bars.
The most commonly reported goal that patients report is to be able to walk again and the GHS allows for early gait training in a safe environment to progress patients quickly out of the parallel bars and improve overall endurance. I would also recommend a trial with the GHS to work on balance training if a patient is having frequent falls at home.
In general, I do not have enough experience to comment on the area of psychological benefits with our active duty/veteran population, but the GHS may reduce anxiety/fear of falling and improve motivation.
–Debbie Pitsch PT, Palo Alto Polytrauma Rehabilitation Center, VA Palo Alto Health Care System, Palo Alto CA
J.T. is a T11/12 incomplete 15 years post. He sustained both an SCI and above knee amputation secondary to a MVA. When he started the program a little over a year ago at RIM, he had a wood prosthetic that was for static standing only. He had not tried to walk in 15 years. His therapist has progressed using the Gait Harness System (GHS) through 2 prosthetics/orthotics to a carbon fiber KAFO with stance control knee and friction knee prosthetic. He has progressed to ambulation with a standard walker plus stand by assistance for safety. He currently is up to 1500 feet in the GHS and 600 feet with a rolling walker. The therapist chose this individual because of the complexity and the ease of application of the GHS with both a prosthetic and orthotic.
A.B. is a C6 complete who had been non-ambulatory for over 10 years. She walks in the GHS with carbon fiber KAFO’s. She only requires assistance for guidance of the GHS. This would require more that one person without the GHS.
B.S. is a 6 foot 5 inch C5 ASIA B status post diving accident. His therapist has progressed him from KAFO’s to AFO’s. Additionally, the therapist has FES applied to the tib anterior and pernoneals that he activates via a trigger switch to break the extension spasticity. The GHS frees up an individual to manually correct improper foot placement. The therapist reports the harness works very well with the braces. This particular individual also buckles on occasion. Generally, this happens when the patient accidentally activates the e-stim bilaterally. The main point is that the GHS effectively prevents him from falling and there is no pain or skin irritation from the harness. The therapist reports this client has tried numerous harnesses and said the GHS harness and the Crawl2@Walk crawling harness is by far the most comfortable.
E. is a T6 complete. He now requires minimal assistance for guidance of the GHS. He currently wears carbon fiber KAFO’s with stance control knees. The Gait Harness works great with the braces.
C.H. is a C6 complete. She is status post MVA in 2002, and nasal tissue stem cell surgery in 2005. She has therapy 3 x wk. In therapy, C.H. can walk 134 feet around a track with leg braces and the GHS, with help from her therapist.
L.B. is a C8 tetraplegic, ASIA A, status post MVA 10 years ago. She attends therapy 3 x wk, 3 hours per session. L.B. uses bilateral carbon fiber stance control KAFOs and a GHS. The two products work together to provide L.B. the opportunity to safely ambulate with a natural reciprocating gait pattern. Since her accident, she has regained some movement and sensation below the level of her injury, much occurring since she started in the SCI program. L.B. has purchased a GHS to be used at home along with the braces. Her husband assists her with a sit to stand into the GHS. Her home therapy program includes neuromuscular E-Stim of all major muscle groups below the lesion level every other day, and standing in the KAFOs and GHS to work on endurance, pre-gait and gait activities.
A.F. is a T8 complete, status post MVA in 2002, and nasal tissue stem cell surgery in 2005. A.F. participated in a SCI program post stem cell surgery. Prior to surgery, she was using non-stance controlled leg braces. Therapy was 3 hours daily. She is currently using stance controlled KAFOs, which allow her legs to move independently within the GHS. The GHS forces her to place most of her 122 pounds on her legs instead of her arms. She is currently progressing by doing therapy at home, walking with the GHS daily.
55 y/o with SCI and LE paralysis went from walking 5 minutes moderate to maximal assistance in the parallel bars to 45 minutes in the GHS independently after 1 week. After one month of therapy, he had improved lower extremity circulation and substantially reduced risk of having his legs amputated secondary to circulatory dysfunction.
K.M. is a 35 y/o male who sustained a TBI as an 11 y/o child, status post MVA 24 years ago. He had been wheelchair bound for 22 years at the time he first began using the GHS in an adult day center program. K.M. began using the GHS 2 years ago, but required 4-person assist and walked just a few steps. He had moderate to severe tremors, and was barely able to stand. Therapy has typically been 2 x week. One year later, he had decreased to a 2 person assist, and was able to routinely walk up to 200 feet in the GHS. This current year, he is down to just a 1 person assist with ambulation in the GHS, and is routinely walking 800 feet per therapy session. His initial focus in therapy was on distance and endurance. Now, he is also focusing on improving his technique and self-correction of form. He is finding it easier to transfer into the GHS. K.M. is showing more stride confidence. He is now able to look at pictures in hallways while walking. Tremors are decreasing, and he is increasing control of his upper torso, head and neck while walking. He is taking less frequent rest stops and finding it easier to initiate initial stepping. Staff members encourage him to bring his shoulders backward, tilt hips and pelvis forward, and take smaller steps. His thigh muscle mass and strength have increased so much he now requires a larger gait harness. K.M.’s home caregiver reports he is much stronger and better able to assist her with transfers at home. After seeing his steady improvement, staff and other program participants are highly motivated to use GHS for a variety of gait and balance dysfunctions.
P.D. sustained a TBI 8 years ago and is a long-term resident. He has very little trunk stability so needs to walk with some assistive device or he loses his balance. He has developed bad habits over the last 8 years. When he walks, the therapist has been teaching him to ambulate within the GHS upright and to correct gait deviations. His progress is much slower, but he is able to walk with more control and stability within the system.
S.B. sustained a TBI in June 2003. This patient has been seen for a couple of weeks and already has progressed out of the GHS and now walks with a rolling walker. He is now able to transfer and walk independently with the walker around the unit. The therapist was able to work with his balance deficits and he was able to regain his balance very quickly. The therapist also has placed resistance tubing around the thigh cuffs for resistance training. Second Step suggested beginning higher level balance training with ball toss and cone activities as a progression to patient’s program.
TBI/CVA patient with severe extensor tone and was totally dependent with standing and ADL’s. Patient has progressed to a level of min. to moderate assistance with sit to stand with bed mobility. The GHS has allowed the therapist to work on static strengthening/balance to foot placement with gait retraining and now the patient is walking 400’ with min-mod assistance. Both OT and PT working with this patient have stated that the GHS has made progress possible for this patient and without it progress would have been minimal.
60 y/o retired MD secondary to Parkinson’s Disease had substantial improvement in gait with reduced falls and improved gait pattern after 1 month of skilled therapy using the GHS.
55 y/o with SCI and LE paralysis went from walking 5 minutes moderate to maximal assistance in the parallel bars to 45 minutes in the GHS independently after 1 week. After one month of therapy, he had improved lower extremity circulation and substantially reduced risk of having his legs amputated secondary to circulatory dysfunction.
25 y/o with TBI from overdose had significant improvement in overall balance and coordination patterns. She had significant dyskinesia that made ambulation a high risk. In the GHS she was low risk of injury to herself and to the treating therapist.
D.H., a bilateral amputee patient in the nursing home setting had substantially improved gait pattern with orthoses and shortened rehab stay while reducing the risk of falls while in the GHS.
65 y/o with a history of a CVA and bilateral TKA had return of functional gait and became independent with a cane after 2 months of rehab one hour per day, three days per week using the GHS and performing neuromuscular re-education activities.
34 y/o male who sustained a TBI in 1994. Patient was at the Tampa VA for therapy from 1996-1997 and recently returned in 2003 for a re-evaluation and was trained in the GHS. The family was educated in the proper set-up and application of the GHS and a request was made to have a unit shipped to Tennessee for patient to use in the home for continuity of care and continued functional training. This patient uses GHS daily at home.
Press Releases
The Headliner, Newsletter of the Brain Injury Alliance of Oregon, Summer 2019, “Second Step spotlights Grace Center for Adult Day Services: State-of-the-art services, thriving participants” – Read here
The Headliner, Newsletter of the Brain Injury Alliance of Oregon, Spring 2017, “Post TBI, Young Father is Overjoyed to Walk Again” – Read here
The Headliner, Newsletter of the Brain Injury Alliance of Oregon, Summer/Fall 2015, “Physical Therapy Assistant takes the next step in his post stroke brain recovery” – Read here
Stroke-Network.com, The Center for Stroke Recovery, Fall 2012, “Gait Harness System Provides Alternative for Mobility Rehabilitation” Read here
Eugene Magazine, Spring 2011, “Step by step” Read here
The Headliner, Newsletter of the Brain Injury Association of Oregon, Spring 2011, “Learning How to Walk Again…And What Better Way to Accomplish Medicaid Spend Down?” Read here
Rehab Management, June 2009, “On the Market: A look at the latest cutting-edge products in the industry-New Gait Harness System” Read here
HME Today, December 2008, “Product Profiles-Gait Harness System” Read Here
Rehab Management, December 2008, “Significant Strides” Read here
Rehab Management, October 2008 , “On the Market: Total Transfer Gait Harness System” Read here
Discovery Health Channel, September 2008, “Medical Incredible” feature View segment here
PT Products Magazine, June 2008, “Aiming High–Setting Ambitious Goals for Those Who Suffer from TBI” Read here
The Headliner, Newsletter of the Brain Injury Association of Oregon, Spring 2008, “A New Approach to Walking Again for Those Living with TBI” Read here
Grace Center for Adult Day Services Newsletter, April 2008, “Director’s Corner: Using the ‘Second Step’ ” Read here
The Headliner, Newsletter of the Brain Injury Association of Oregon, Summer 2007, “New Hope for Those Living with Traumatic Brain Injuries: Learning to Walk Again” Read here
Detroit Free Press, January 2007, “A Chance to Walk Again” Read here
Whittier Rehab Hospital’s Rehabilitation Today, Vol. 3 Issue 3, 2006/2007, “On the Road to Recovery-The Story of Ron Guilette” Read here
Rehabbing Rehabilitation, Therapy Times, September 2006, “Physical Therapy-Overcoming Obstacles with a Dual Product Approach” Read here
Detroit Free Press, November 2005, “Technology charges forward” Read here
CBS Today Show interview, June 2003, Read here
Nursing Homes Magazine, October 2000, “Therapy Support Device” Read here
Clients need to practice safe standing and walking again much more than limited weekly therapy clinic sessions can provide. Motor learning suggests that practice, repetition and task specificity are instrumental to task improvement in learning to stand and walk again.
Extending the practice of therapeutic activities beyond the clinical environment and into the home is a great way to apply these principles and reinforce the gains made in the clinic. The Second Step Gait Harness System for Home Users, all-in-one standing frame and walking frame, fills that therapy gap, providing comfortable, at home ability to work on the tasks of learning to stand and walk again.
Contact Us Today
We are here to help you
For personalized attention, please call or email us today. We will take the time to answer all your questions about how the Gait Harness System is helping people walk again, and whether it could be right for you.
We will do our best to respond to your request within 24 hours, or on the next business day. All information you provide is strictly confidential and will never be sold or shared with any other person, entity or organization. See our Privacy Policy.
Office hours
Monday – Thursday
9:00 am – 5:00 pm ET
Friday
9:00 am – 3:00 pm ET
Sales Office and Support
P.O. Box 565
Anna Maria, FL 34216-0565
Phone: 941.567.4200
Toll Free: 877.299.STEP (7837)
Fax: 877.299.5428





